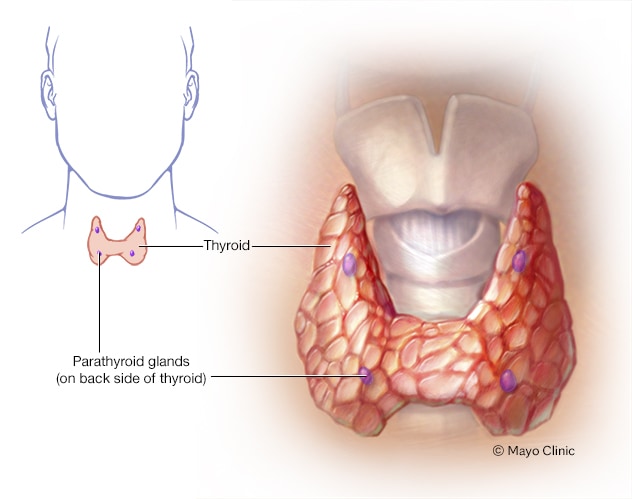
"Hyperparathyroidism is an excess of parathyroid hormone in the bloodstream due to overactivity of one or more of the body's four parathyroid glands. These glands are about the size of a grain of rice and are located in your neck.
The parathyroid glands produce parathyroid hormone, which helps maintain an appropriate balance of calcium in the bloodstream and in tissues that depend on calcium for proper functioning.
Two types of hyperparathyroidism exist. In primary hyperparathyroidism, an enlargement of one or more of the parathyroid glands causes overproduction of the hormone, resulting in high levels of calcium in the blood (hypercalcemia), which can cause a variety of health problems. Surgery is the most common treatment for primary hyperparathyroidism.
Secondary hyperparathyroidism occurs as a result of another disease that initially causes low levels of calcium in the body and over time, increased parathyroid hormone levels occur.
Symptoms
Hyperparathyroidism is often diagnosed before signs or symptoms of the disorder are apparent. When symptoms do occur, they're the result of damage or dysfunction in other organs or tissues due to high calcium levels circulating in the blood and urine or too little calcium in bones.
Symptoms may be so mild and nonspecific that they don't seem at all related to parathyroid function, or they may be severe. The range of signs and symptoms include:
- Fragile bones that easily fracture (osteoporosis)
- Kidney stones
- Excessive urination
- Abdominal pain
- Tiring easily or weakness
- Depression or forgetfulness
- Bone and joint pain
- Frequent complaints of illness with no apparent cause
- Nausea, vomiting or loss of appetite
When to see a doctor
See your doctor if you have any signs or symptoms of hyperparathyroidism. These symptoms could be caused by any number of disorders, including some with serious complications. It's important to get a prompt, accurate diagnosis and appropriate treatment.
Causes
Hyperparathyroidism is caused by factors that increase the production of parathyroid hormone.
The parathyroid glands maintain proper levels of both calcium and phosphorus in your body by turning the secretion of parathyroid hormone (PTH) off or on, much like a thermostat controls a heating system to maintain a constant air temperature. Vitamin D also is involved in regulating the amount of calcium in your blood.
Normally, this balancing act works well. When calcium levels in your blood fall too low, your parathyroid glands secrete enough PTH to restore the balance. PTH raises calcium levels by releasing calcium from your bones and increasing the amount of calcium absorbed from your small intestine.
When blood-calcium levels are too high, the parathyroid glands produce less PTH. But sometimes one or more of these glands produce too much hormone, leading to abnormally high levels of calcium (hypercalcemia) and low levels of phosphorus in your blood.
The mineral calcium is best known for its role in keeping your teeth and bones healthy. But calcium has other functions. It aids in the transmission of signals in nerve cells, and it's involved in muscle contraction. Phosphorus, another mineral, works in conjunction with calcium in these areas.
The disorder can generally be divided into two types based on the cause. Hyperparathyroidism may occur because of a problem with the parathyroid glands themselves (primary hyperparathyroidism) or because of another disease that affects the glands' function (secondary hyperparathyroidism).
Primary hyperparathyroidism
Primary hyperparathyroidism occurs because of some problem with one or more of the four parathyroid glands:
- A noncancerous growth (adenoma) on a gland is the most common cause.
- Enlargement (hyperplasia) of two or more parathyroid glands accounts for most other cases.
- A cancerous (malignant) tumor is a rare cause of primary hyperparathyroidism.
Primary hyperparathyroidism usually occurs randomly, but some people inherit a gene that causes the disorder.
Secondary hyperparathyroidism
Secondary hyperparathyroidism is the result of another condition that lowers calcium levels. Therefore, your parathyroid glands overwork to compensate for the loss of calcium. Factors that may contribute to secondary hyperparathyroidism include:
- Severe calcium deficiency. Your body may not get enough calcium from your diet, often because your digestive system doesn't absorb the calcium from it.
Severe vitamin D deficiency. Vitamin D helps maintain appropriate levels of calcium in the blood, and it helps your digestive system absorb calcium from your food.
Your body produces vitamin D when your skin is exposed to sunlight, and you consume some vitamin D in food. If you don't get enough vitamin D, then calcium levels may drop.
- Chronic kidney failure. Your kidneys convert vitamin D into a form that your body can use. If your kidneys function poorly, usable vitamin D may decline and calcium levels drop. Chronic kidney failure is the most common cause of secondary hyperparathyroidism.
Risk factors
You may be at an increased risk of primary hyperparathyroidism if you:
- Are a woman who has gone through menopause
- Have had prolonged, severe calcium or vitamin D deficiency
- Have a rare, inherited disorder, such as multiple endocrine neoplasia, type 1, which usually affects multiple glands
- Have had radiation treatment for cancer that has exposed your neck to radiation
- Have taken lithium, a drug most often used to treat bipolar disorder
Complications
Complications of hyperparathyroidism are primarily related to the long-term effect of too little calcium in your bones and too much calcium circulating in your bloodstream. Common complications include:
- Osteoporosis. The loss of calcium often results in weak, brittle bones that fracture easily (osteoporosis).
- Kidney stones. The excess of calcium in your blood may lead to excess calcium in your urine, which can cause small, hard deposits of calcium and other substances to form in your kidneys. A kidney stone usually causes significant pain as it passes through the urinary tract.
- Cardiovascular disease. Although the exact cause-and-effect link is unclear, high calcium levels are associated with cardiovascular conditions, such as high blood pressure (hypertension) and certain types of heart disease.
- Neonatal hypoparathyroidism. Severe, untreated hyperparathyroidism in pregnant women may cause dangerously low levels of calcium in newborns.
Diagnosis
Blood tests
If the result of a blood test indicates you have elevated calcium in your blood, your doctor will likely repeat the test to confirm the results after you have not eaten for a period of time (fasted).
A number of conditions can raise calcium levels, but your doctor can make a diagnosis of hyperparathyroidism if blood tests show you also have elevated parathyroid hormone.
Additional diagnostic tests
After making a diagnosis of hyperparathyroidism, your doctor will likely order additional tests to rule out possible secondary causes, to identify possible complications and to judge the severity of the condition. These tests include:
Bone mineral density test (bone densitometry). The most common test to measure bone mineral density is dual energy X-ray absorptiometry (DXA).
This test uses special X-ray devices to measure how many grams of calcium and other bone minerals are packed into a segment of bone.
Urine test. A 24-hour collection of urine can provide information on how well your kidneys function and how much calcium is excreted in your urine.
This test may help in judging the severity of hyperparathyroidism or diagnosing a kidney disorder causing hyperparathyroidism. If a very low level of calcium in the urine is found, this may indicate a condition that doesn't require treatment.
- Imaging tests of kidneys. Your doctor may order X-rays or other imaging tests of your abdomen to determine if you have kidney stones or other kidney abnormalities.
Imaging tests before surgery
If your doctor recommends surgery, he or she will likely use one of these imaging tests to locate the parathyroid gland or glands that are causing problems:
Sestamibi parathyroid scan. Sestamibi is a radioactive compound that is absorbed by overactive parathyroid glands and can be detected by a scanner that detects radioactivity.
The normal thyroid gland also absorbs sestamibi. To eliminate uptake in the thyroid obscuring the uptake in a parathyroid adenoma, radioactive iodine, which is only taken up by the thyroid, also is given and the thyroid image is digitally subtracted.
Computerized tomography (CT) scanning may be combined with the sestamibi scan to improve detection of an abnormality.
Ultrasound. Ultrasound uses sound waves to create images of your parathyroid glands and surrounding tissue.
A small device held against your skin (transducer) emits high-pitched sound waves and records the sound wave echoes as they reflect off internal structures. A computer converts the echoes into images on a monitor.
Treatment
Watchful waiting
Your doctor may recommend no treatment and regular monitoring if:
- Your calcium levels are only slightly elevated
- Your kidneys are functioning normally, and you have no kidney stones
- Your bone density is normal or only slightly below normal
- You have no other symptoms that may improve with treatment
If you choose this watch-and-wait approach, you'll likely need periodically scheduled tests to monitor your blood-calcium levels and bone density.
Surgery
Surgery is the most common treatment for primary hyperparathyroidism and provides a cure in about 95 percent of all cases. A surgeon will remove only those glands that are enlarged or have a tumor (adenoma).
If all four glands are affected, a surgeon will likely remove only three glands and perhaps a portion of the fourth — leaving some functioning parathyroid tissue.
Surgery may be done as an outpatient procedure, allowing you to go home the same day. In such cases, the surgery can be done through very small incisions in the neck, and you receive only local anesthetics.
Complications from surgery aren't common. Risks include:
- Damage to nerves controlling the vocal cords
- Long-term low calcium levels requiring the use of calcium and vitamin D supplements
Drugs
Medications to treat hyperparathyroidism include the following:
Calcimimetics. A calcimimetic is a drug that mimics calcium circulating in the blood. The drug may trick the parathyroid glands into releasing less parathyroid hormone. This drug is sold as cinacalcet (Sensipar).
The Food and Drug Administration approved cinacalcet to treat hyperparathyroidism caused by chronic kidney disease or parathyroid cancer. Some doctors may prescribe it to treat primary hyperparathyroidism, particularly if surgery hasn't successfully cured the disorder or a person isn't a good candidate for surgery.
The most commonly reported side effects of cinacalcet are joint and muscle pain, diarrhea, nausea, and respiratory infection.
Hormone replacement therapy. For women who have gone through menopause and have signs of osteoporosis, hormone replacement therapy may help bones retain calcium. This treatment doesn't address the underlying problems with the parathyroid glands.
Prolonged use of hormone replacement therapy can increase the risk of blood clots and breast cancer. Work with your doctor to evaluate the risks and benefits to help you decide what's best for you.
Some common side effects of hormone replacement therapy include breast pain and tenderness, dizziness, and headache.
- Bisphosphonates. Bisphosphonates also prevent the loss of calcium from bones and may lessen osteoporosis caused by hyperparathyroidism. Some side effects associated with bisphosphonates include low blood pressure, fever and vomiting.
Lifestyle and home remedies
If you and your doctor have chosen to monitor, rather than treat, your hyperparathyroidism, the following suggestions can help prevent complications:
Monitor how much calcium and vitamin D you get in your diet. Restricting dietary calcium intake is not advised for people with hyperparathyroidism. The Institute of Medicine recommends 1,000 milligrams (mg) of calcium a day for adults ages 19 to 50 and men ages 51 to 70. That calcium recommendation increases to 1,200 mg a day for women age 51 and older and men age 71 and older.
The Institute of Medicine also recommends 600 international units (IUs) of vitamin D a day for people ages 1 to 70 and 800 IUs a day for adults age 71 and older. Talk to your doctor about dietary guidelines that are appropriate for you.
- Drink plenty of fluids. Drink enough fluids, mostly water, to produce nearly clear urine to lessen the risk of kidney stones.
- Exercise regularly. Regular exercise, including strength training, helps maintain strong bones. Talk to your doctor about what type of exercise program is best for you.
- Don't smoke. Smoking may increase bone loss as well as increase your risk of a number of serious health problems. Talk to your doctor about the best ways to quit.
- Avoid calcium-raising drugs. Certain medications, including some diuretics and lithium, can raise calcium levels. If you take such drugs, ask your doctor whether another medication may be appropriate for you.
Preparing for your appointment
In most cases, elevated calcium is detected by blood tests your doctor has ordered as part of a routine screening, a diagnostic work-up for an unrelated condition or a diagnostic work-up to identify the cause of very general symptoms.
Talk to your doctor about test results if they show you have high levels of calcium. Questions you might ask your doctor include:
- Do I have hyperparathyroidism?
- What test do I need to confirm the diagnosis or determine the cause?
- Should I see a specialist in hormone disorders (endocrinologist)?
- If I have hyperparathyroidism, do you recommend surgery?
- What alternatives do I have to surgery?
- I have these other health conditions. How can I best manage them together?
- Do you have printed material about hyperparathyroidism that I can take home?
To understand the effect of hyperparathyroidism on your overall health, your doctor may ask you questions about possible mild signs or symptoms, including:
- Have you been feeling depressed?
- Do you often feel tired, easily fatigued or generally unwell?
- Are you feeling any inexplicable aches and pains?
- Are you often forgetful, absent-minded or unable to concentrate?
- Have you experienced increased thirst and excessive urination?
Your doctor may ask you additional questions about what medications you're taking and what your diet is like to help determine if you get adequate amounts of calcium and vitamin D."
Finally, here is an article (with additional info) from WebMD:
Your body needs calcium from head to toe. But there are times when your body can have so much calcium that it’s not good for you. A condition called hyperparathyroidism can cause such a situation to happen, where your levels of calcium in your blood and tissues are too high. And it has nothing to do with how much milk you drink.
In your neck, there are four similar glands -- each about the size of a grain of rice -- called parathyroid glands. They make a hormone that helps keep your amount of calcium at just the right level. But when even one of those glands makes too much of the hormone, the result is hyperparathyroidism.
The hormone, called parathyroid hormone, has three ways it can raise your calcium level: It can tell your bones to release some calcium, tell your small intestine to absorb more calcium into your bloodstream, or tell your kidneys to hang on to more calcium instead of sending it out of your body in your pee.
Types
There are two kinds of hyperparathyroidism:
Primary. This means that your condition is caused by, or starts in, at least one of the parathyroid glands naturally making too much of the hormone that keeps your calcium levels in balance.
Secondary. This means that some other disease or condition is to blame. The common trigger is low calcium levels in the
blood, which prompts your body to release parathyroid hormone almost immediately.
How Common Is It?
About 100,000 people in the U.S. develop this condition each year. People between the ages of 50 and 60, and women, are the most likely to have hyperparathyroidism.
Causes
Primary hyperparathyroidism can happen due to:
A noncancerous tumor in one of the parathyroid glands. This causes most primary cases.
Two or more of the glands being too active and producing too much of the parathyroid hormone.
Cancer of one of the glands. This is a very rare cause of primary hyperparathyroidism.
Secondary hyperparathyroidism (apart from kidney failure) can happen if:
Your body doesn’t get enough calcium. You could have low calcium levels in your blood for different reasons. You might be too low on vitamin D, or your digestive system might have problems with absorbing calcium. It also often happens if you have chronic kidney disease.
You have extremely low levels of vitamin D. This vitamin helps balance the amount of calcium in your blood, and it helps your digestive system absorb calcium.
Symptoms
If you have primary hyperparathyroidism, you most likely don’t have any symptoms. But if you do have symptoms, they are likely not severe. They include:
- Muscles that feel weaker than usual
-
Fatigue and wanting to sleep more
-
Pain in your joints and bones
-
Depression
But if you have a more severe form of primary hyperparathyroidism and your calcium levels rise, your symptoms also could include:
- Being constipated
- Feeling nauseated
- Throwing up
- Not feeling hungry
- Feeling confused or forgetting things
- You’re more thirsty than usual
- You pee more often than normal
- You have pain on one side of your lower abdomen (if you have kidney stones)
Diagnosis
Your doctor will make the diagnosis based on blood tests.
If the results show that you have high levels of parathyroid hormone and of calcium, then you have primary hyperparathyroidism. You’ll then get:
- X-rays to check for broken bones in certain areas, including in your back
-
Bone density tests to look for reduced bone mineral density, especially in your forearm
- Kidney ultrasound to look for kidney stones
- 24-hour urine calcium collection to check for any kidney problems
Blood tests looking at how well your kidneys work and your levels of phosphate and vitamin D can suggest secondary hyperparathyroidism.
Treatment
If you have secondary hyperparathyroidism, your doctor may recommend supplements of vitamin D and calcium.
If you have primary hyperparathyroidism and you have bothersome symptoms, you’ll need surgery to remove the overactive parathyroid gland or glands. For example, if you have extremely high blood calcium levels, have had a broken bone (or fracture), or have kidney stones, your doctor will likely want you to have that operation.
Even if you don’t have symptoms, your doctor may recommend the operation, depending on how you together decide to treat the condition.
You might get these benefits from the surgery:
- Improved bone density
- Fewer bone fractures
- Less chance of forming kidney stones
Surgery cures primary hyperparathyroidism in 95% of cases. Choose a surgeon who has a lot of experience in parathyroid surgery. Like any operation, there can be complications, so talk with your doctor about the risks and benefits, what to expect during the recovery, and how long you’ll be in the hospital.
If you’re not a candidate for surgery, you might just need:
- Routine exams by your doctor
- Blood tests
- Bone density tests
Living With Hyperparathyroidism
If you and your doctor decide you don’t need the surgery, you can:
Track how much vitamin D and calcium you get through your diet. But don’t deliberately cut down on calcium. Talk to you doctor about whether you should take supplements, and if so, how much.
Drink lots of fluids, especially water. Enough water can help prevent kidney stones
Exercise
. Regular exercise, especially strength training, keeps your bones strong.